
I have come to learn that having a practitioner that you can partner with – one who can draw from a vast depth and breadth of knowledge, provide profound healing sessions all the while giving you the tools and suggestions to live well– is crucial in staying healthy, flexible, and active.
Dr. Seo is the cornerstone of my wellness program. We are SO VERY FORTUNATE to have such a gifted practitioner in our community. I cannot thank him enough.
Sandy M.
TMJ / TMD
Are you suffering from jaw pain, clicking, or locking while eating, talking or yawning? Does the side of your head, face, and jaw hurt in the morning and towards end of the day? These are the most common complaints of TMJ disorders. TMJ pain can occur by a traumatic incident such as falling on the chin or a whiplash from a motor vehicle accident. But in most cases, it’s due to gradual wear and tear, and lack of maintenance. In many cases, patients will deal with annoying jaw clicking for a long period of time. It may hurt on an occasion but pain typically goes away. And one day, the pain gets excruciating worse from a simple daily movement such as eating or yawing.
The jaw may lock and it needs to be shifted to the side to re-open and close. Some patients have been told by their dentist that they clench at night; therefore, wear a night guard clenching still occurs. Unfortunately at this point, degeneration of TMJ has already begun. But have hope. We have been successfully treating people with these problems without medications or surgery by addressing the underlying problems rather than treating symptoms. Becoming pain free is easier than you think. Fill out the simple form below and get back to doing what you love.
Temporal Mandibular Joint (TMJ) Disorder Explained
TMJ Disorder is a condition that can cause clenching, pain, and clicking in the jaw and muscles that control the jaw movement. An estimated 75% of the U.S. population has experienced one or more signs of TMJ Disorder. Most TMJ Disorder symptoms are temporary, but 10% of the population will require professional treatment. The condition appears to be more common in women than men. TMJ Disorders involve more than a single symptom and involve multiple causes. The pain may arise suddenly or progress over a period of months to years with intermittent frequency and intensity. The most successful and scientifically supported treatment consists of conservative therapy, which shows that over 50% of TMJ Disorder patients have few or no symptoms.
What is TMJ and TMJ Disorder?
TMJ is an orthopedic joint that connects the mandible (lower jawbone) to the temporal bone of the skull in the front of the ear. The disc cushions the load between the two bones while the jaw opens. Any problem that prevents this complex system of muscles, ligaments, discs and bones from working properly will result in painful TMJ disorder. TMJ Disorder includes the jaw joint, muscles, tendons, ligaments, and nerves.
Symptoms of TMJ Disorder
- Headaches
- Pain behind the eyes or blurring of vision
- Unexplained tooth pain
- Earaches, congestion or ringing in ears
- Clicking, popping or grating sound in the jaw
- Limited opening or locking of the jaw
- Dizziness
- Pain with chewing
- Facial pain and/or numbness of face and head
- Neck pain
- Throat discomfort
- Difficulty in closing the teeth together
Causes of TMJ Disorder
- Poor posture
- Lack of neck and upper back movement
- Tight facial and mouth muscles
- Trigger points
- Trauma or whiplash
- Malignment of teeth and bite (malocclusion)
- Clenching or grinding
- Mouth breathing
- Stress
- Habits such as nail biting, gum chewing, frowning, etc.
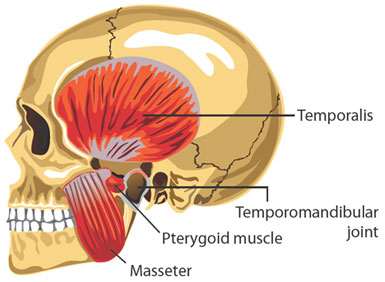
Muscles of the TMJ
Muscles of mastication (jaw muscles) connect the mandible (lower jaw) to the maxillae (upper jaw), skull, and neck. These muscles open close, protrude, and move the jaw side to side, enabling you to talk, chew, and swallow. The supporting muscles of mastication consist of neck and shoulder muscles and these muscles stabilize the skull on the neck during jaw function.
TMJ Mechanics
The TMJ is a “loose-fitting”, rotating and sliding joint with a fibro-cartilage covered, football shaped ball (condyle), fibrous pad (disc), fibro-cartilage lined socket (fossa), ligaments, tendons, blood vessels, and nerves. The fibrous pad/disc functions as a moving shock absorber and stabilizer between the condyle and fossa. As the jaw opens, the condyle rotates and slides forward with the disc.
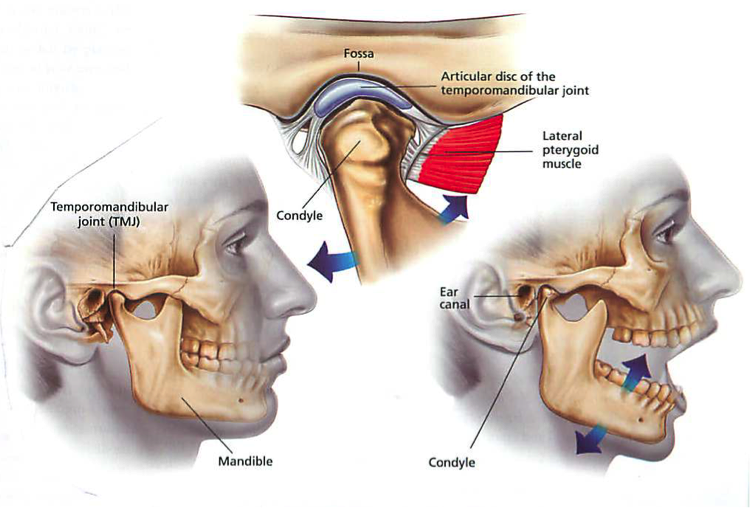
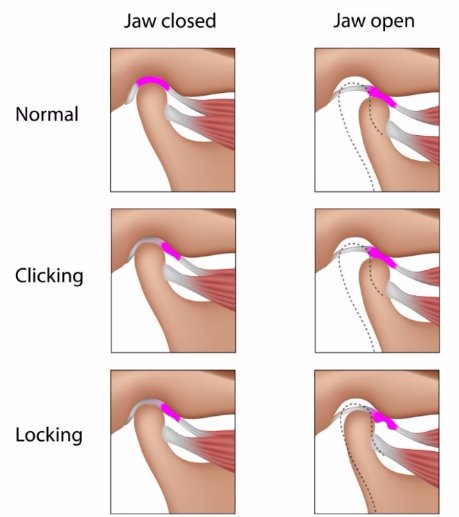
Normal TMJ Movement
In a normal TMJ movement, the disc is between the condyle (jaw joint) and the temporal bone. It provides cushion and allows the condyle to glide along the temporal bone. Without this cushion, the two bones will wear each other down causing degeneration of the bones and pain. As the jaw opens, the disc stays between the condyle and temporal bone.
Jaw Clicking or Popping
A jaw that pops or clicks when opening and/or closing, is an indication of a TMJ disorder. When the upper and lower teeth are together, the disc is not between the jaw joint. This may cause ringing, stuffiness or fullness of the ears, earaches, temple pain, and/or facial pain. TMJ pain can also occur with clicking or popping, but many times pain is not experienced.
Jaw Locking
Lockjaw or Closed Lock is the termed used for a TMJ disorder in which the disc is not between the jaw joint and the disc does not slip back onto the jaw joint when opening the mouth. Opening of the mouth is limited by half of normal range.
The upper & lower teeth are together and the disc is off the jaw joint (condyle). This may cause ringing, stuffiness or fullness of the ears, earaches, temple pain and/or facial pain. TMJ pain is experienced by many people when a TMJ disorder advances to this stage. The disc can be placed back onto the jaw joint, especially if treated early after onset. If treatment is not done, degeneration of the TMJ may occur causing more pain and dental problems.
Advanced Stage of TMJ Disorder
TMJ disorders can progress to degeneration of the joint and surrounding tissues. Bone, ligaments and disc deterioration can occur if TMJ disorders are left untreated. In worse cases, surgery is warranted.
Evaluation of TMJ Disorder
A comprehensive history is necessary to understand the characteristics of the symptoms. Para-functional activities, such as grinding, thumb sucking, biting nails, chewing gum, or tongue thrusting, can all cause or create TMJ disorders and dramatically affect the direction of growth and development that can permanently affect one’s lifelong appearance and ability to function normally. Emotional stress, work position, posture, sleeping position, reading, electronic usage, and hobbies may be exacerbating the symptoms. Clicking of the jaw, neck pain and headaches frequently occur with patients that suffer from TMJ Disorders. And it may progress to facial and ear symptoms. It may be described as mild or severe and dull or sharp and better or worse with certain physical movements. These characteristics will help localize the issue and point towards the root of origins.
A thorough physical examination from head to toe is key to understanding the cause of the TMJ Disorder. This process typically includes the following:
- Observing symmetry of the face, specifically the eyes, nose, mouth, chin and jaw line.
- Alignment of the teeth, noting symmetry, close bite, under bite and over bite.
- Overall posture is observed for forward head posture, rounded shoulders, scapular protraction, and pelvis rotation.
- Measuring range of motion of the jaw as it opens and closes, side to side and forward. At the same time, listening for noises such as clicking, popping or grinding helps to paint the clinical picture.
- Assessing tongue or lip frenulum restriction, which may limit the ability to open the mouth at a normal range.
- Test the motor function and strength of the muscles of mastication (chewing), along with deep cervical flexors (core neck muscles), and scapular stabilizers (shoulder muscles).
- Sensory function is tested to look for areas of numbness, tingling or burning, specifically the upper quadrant dermatomes, C1, C2, C3, cutaneous nerve supply of the face, scalp and neck, and cranial nerves V – XII.
- Reflex of the jaw called the Jaw Jerk Reflex is tested to provide insight to the connection of nerve, spinal cord and muscle.
- Range of Motion and muscle length of the cervical spine is tested to determine if nerve, spinal cord or pain emerges.
- Joint capsule mobility of the TMJ and cervical spine is performed to identify pain and mobility dysfunction.
- Palpation of the muscles of mastication including the temporalis, masseter and pterygoids is performed to assess for trigger points or tendonitis.
- Observing breathing patterns help to determine if the patient is utilizing diaphragmatic breathing, using accessory muscles or is a mouth breather.
Treatment
A clinician who focuses their practice and treatments on TMJ disorder is uniquely qualified to effectively treat the cause of the pain and discomfort. Long term follow up studies of TMJ Disorder patients show that up to 90% of patients have few or no symptoms after conservative treatment. A comprehensive examination will identify and reduce contributing factors to the neuro-musculoskeletal problems, reduce inflammation, restore function and promote repair and regeneration of injured tissues. The first visit should consist of a comprehensive examination of the whole body, not just the TMJ, followed by education of the diagnosis, plan, manual treatment and postural education.
Based on the examination, treatments may consist of the following:
- Manual joint mobilization will restore joint mechanics which leads to improved function and decreased TMJ pain. Mobilization of the TMJ is a highly skilled passive movements that are applied at varying speeds and amplitudes.
- Myofascial and soft tissue release is performed to break the adhesion within muscles, tendons, and fascia. Increased mobility prevents compression and promotes normal mobility and flexibility of the body’s connective tissues. This will help to reduce inflammation, sensitivity, and TMJ pain.
- Posture training for the neck, back, shoulder, and tongue. Correct rest position of the tongue, jaw, neck and back allows for optimal physiological state of interaction between the jaw and the rest of the body.
- Diaphragmatic breathing is important to reduce respiratory dysfunctional mechanics. Excessive use of accessory breathing musculature contributes to TMJ and neck pain.
- Implementing a neuromuscular exercise program and proper posture tends to be the best prevention for TMJ Disorders. For jaw muscles, exercises are not so much for enhancing power and strength, but instead for promoting better neuromuscular stability and motion. To support the jaw, postural muscles in the neck and shoulders will need to be balanced from the front and back of the spine. This phase of treatment is crucial to promote patient’s independence and maintain the benefits of manual treatments.
- Professional instructions and directed progression is key to recovering quickly without setbacks.
- In most visits, a minimum of half of visits should consist of manual treatment and visits should not consist of repetitive exercises that can be performed independently at home.

